Edited by Ana-Maria Oproescu
This is a summary of a research study conducted by ICORD Principal Investigators Dr. Brian Kwon, Dr. Jordan Squair, Dr. Scott Paquette, Dr. Marcel Dvorak, Dr. Christopher West, and colleagues.
To read the original research paper, please click here.
Recent research has shown that an individual’s spinal cord perfusion pressure immediately after spinal cord injury (SCI) is associated with their subsequent neurological recovery.
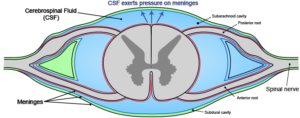
Spinal cord perfusion pressure (SCPP) is the difference between mean arterial pressure (MAP) and cerebrospinal fluid pressure (CSFP). Mean arterial pressure is the pressure exerted on blood vessel walls leaving the heart, and cerebrospinal fluid pressure is the pressure exerted on the meninges (protective coverings) of the brain and spinal cord by spinal fluid.
After someone is admitted to the hospital following an acute SCI, their MAP is maintained at 85-90 mm Hg by doctors for up to a week. Maintaining the MAP at this level is the current recommendation from clinical practice guidelines. The authors of this paper noted, however, that for traumatic brain injury, doctors monitor the intracranial pressure (instead of MAP) so that they can then calculate and monitor the cerebral perfusion pressure. Why is a similar practice not in place for SCI?
This group of researchers decided to investigate how monitoring CSFP in the lumbar spine after SCI relates to neurological recovery.
How was this longitudinal study conducted?
This study involved monitoring 92 individuals with acute SCI from numerous locations across Canada, for one week after sustaining an injury. People enrolled in the study had A, B, and C level injuries on the ASIA (American Spinal Injury Association) Impairment Scale. These individuals had both MAP and CSFP measured using arterial (placed within the artery) and intrathecal (placed within the spinal canal) catheters. Individuals also did formal neurological testing to track their neurological recovery. The arterial and intrathecal catheters were kept in place to monitor pressure over five days. The SCPP for each individual was calculated by MAP – CSFP. Six months later, neurological recovery was scored based on upper extremity, lower extremity and total motor recovery. This allowed researchers to measure the relationship between spinal cord perfusion pressure and neurological recovery in each individual.
Is spinal cord perfusion pressure a good predictor of neurological recovery after SCI?
The researchers observed that CSFP above 50 mm Hg during the first five days after injury was predictive of positive neurological recovery six months post-injury. They also saw that neurological recovery (as measured by upper extremity, lower extremity and total motor recovery) was poor when SCPP fell below 50 mm Hg.
The researchers did a statistical analysis, and discovered the optimal level at which SCPP should be maintained in acute SCI patients to increase their chances of positive neurologic improvement. Because SCPP can be indirectly controlled by changing MAP and CSFP, the authors recommend that MAP be kept above 70 mm Hg and the CSFP below 27 mm Hg for the best chance of recovery. Doing this would keep SCPP above 50 mm Hg.
The researchers argue that the SCPP is a more robust predictor of neurologic recovery than the MAP or CSFP.
What do these findings mean for people with SCI?
These results are important as they will help to create guidelines for spinal cord perfusion pressure and how it should be maintained in the hospital after injury to ensure the best possible neurological outcome. Spinal cord perfusion pressure can be modified by either raising mean arterial pressure through medications that constrict the blood vessels, or by lowering cerebral spinal fluid by the draining of excess fluid. This research can help future individuals who sustain a spinal cord injury have the best chance at neurological recovery.
Limitations of this study:
This finding will only be directly applicable to individuals who sustain a SCI in the future, and not to those who are already living with SCI. However, this finding is useful because it may allow doctors to optimize SCPP in future patients in order to better their chances of neurologic recovery. Additionally, this study measured pressure posterior to the injury site, where the pressure might be lower than at the injury site. The present authors chose this approach because it was easier and less risky to insert a catheter into this region.