 | 5 comments
| 5 comments
By Gabrielle John
Research in focus aims to profile and translate research that has been reviewed by highly respected peers in the field of spinal cord injury to the community, as a means to maintain community engagement with on going research.
Stem cells are often grabbing headlines but sadly much of how they are conveyed to the public is misleading. With the recent introduction of Canada’s first national public blood bank for umbilical cord blood (a rich source of stem cells), and the rising popularity of stem cell tourism, it is important for scientists to remain engaged with the public and convey their research in terms the public can understand.
In 2012, researchers from the University of California at Los Angeles (UCLA) and the University of California at San Diego (UCSD) published their research on the regrowth of nerve cells after spinal cord injury using neural (nerve-related) stem cells in the well-respected scientific journal Cell. You can find the original article, Long-distance growth and connectivity of neural stem cells after severe spinal cord injury. Cell 150:1264–1273, here. In this edition of Research in Focus, we will look at what this research means in relation to the field of spinal cord injury (SCI) but also for people with SCI.
In this study, researchers used animals as a model to study the relevance of stem cells in spinal cord injury without causing damage to humans. (For further information regarding the use of animals in research, we recommend you look at the University of British Columbia’s Animal Research page.) The authors of this paper looked at the use of human neural stem cells following a severe spinal cord injury – equivalent to a complete spinal cord injury at the 3rd thoracic vertebrae, between the shoulder blades in a human. Injuries like this in a human would result in the complete loss of mobility and sensation below the upper chest, and cause pain, muscle spasms and loss of bladder, bowel and sexual function. Stem cells have the ability to become a variety of other types of cells, such as nerve cells, making them a useful tool in regenerating new tissue in areas of disease or injury, such as SCI.
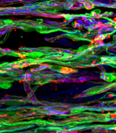
In this study, the researchers used neural stem cells (stem cells that have the capacity to become nerve tissue such as that found in the spinal cord) and embedded them in an engineered substance called a fibrin matrix, used to help support living tissue. This fibrin matrix increases the survival of the stem cells once they have been transplanted into the spinal cord. In addition, a number of different growth factors, proteins that aid survival and growth of these cells, were also embedded in the fibrin matrix. The authors noticed that the transplanted cells were able to become a number of different cell types, including neurons, and showed good survival, a common obstacle in cell transplantation. Another difficulty with transplanted cells can be their inability to grow or move away from the injury site. However, these transplanted stem cells were able to grow long distances beyond the injury and in both directions, towards the brain and towards the tailbone.
An important question following this work was whether or not these transplanted cells could form connections and communicate with other cells found normally within the body. By placing a stimulating electrode, which delivers an electrical signal, above the injury and a recording electrode below the injury, the researchers found that the transplanted cells could act as a relay and pass along information coming from the brain to the rest of the body (communication that would otherwise be disrupted due to the SCI). However, just because these cells were able to pass this information along to other cells did not necessarily mean they could improve functional recovery, so the authors assessed the animals’ behaviour and looked at whether these transplanted cells could improve their ability to move their hindlimbs after the spinal cord injury. Although there was a significant improvement in the hindlimb movement of animals that had received the cell transplant, it was not enough to allow them to support their own weight.
This study showed promising results with regard to the use of stem cells, however, there are some limitations. One concern with this method is the use of numerous growth factors, a fibrin matrix and stem cells. Despite the possible necessity of a combined approach for future treatments of SCI, it is difficult to distinguish which element is responsible for the effect seen. Was the growth witnessed by the authors due to the numerous growth factors put in the spinal cord? If so, which growth factor allowed the cells to grow best? Finding answers to these questions could take years, but will be essential to the development of safe, effective treatments for SCI at some point down the line.
Another item to consider is that the results obtained from animal models can differ significantly from those seen in humans and that the translation of these results into the human context can take a significant length of time. Stem cells offer hope and have tremendous potential to become therapies for SCI in the future but it is important to remember the need for a rigorous, evidence-based approach when developing and applying such therapies. As long as inappropriate hype continues to surround the topic of stem cells, open communication between the community and researchers is key in preventing the propagation of this type of misinformation.

