Welcome to the fifth issue of the ICORDian community newsletter. In this issue, we introduce you to some new researchers, tell you about some interesting new studies, provide a perspective on a new therapy that’s been in the news, and show you some great photos. Plus: a new column by PhD student Jessica Inskip and exciting news from SCI-BC and RHI.
- New PIs
- Innovations in telehealth
- Royal presentation
- Dr. Brian Kwon leads a new project
- SCI in the news
- View from the bench
- Shall we dance
- Gala preview (what does funding support?)
- Partner news
Brain Gain: ICORD gets two new researchers
ICORD has two new Principal Investigators: Drs. Christopher West and John Kramer are both Michael Smith Foundation for Health Research Scholars, jointly funded by the Rick Hansen Institute.
Dr. West is a new Assistant Professor in the UBC School of Kinesiology. He completed in PhD in England investigating cardiorespiratory function and exercise performance in athletes with spinal cord injury (SCI). In 2011, he joined Dr Krassioukov’s laboratory as a post-doc to investigate mechanisms of disordered cardiovascular control after experimental SCI. He has published more than 20 papers in the field of SCI, conducted research at the last 3 Paralympic Games, and has received numerous accolades for his work. In his new position his lab will take a translational approach to investigate mechanisms of cardiac and vascular decline after spinal cord injury.
Like Dr. West, Dr. Kramer is also a new Assistant Professor in the UBC School of Kinesiology. He has a BSc in Kinesiology from the University of Calgary, an MSc in Neuroscience from UWO, and a PhD in Neuroscience from UBC, which he completed with Drs. Armin Curt and John Steeves. Dr. Kramer completed 2.5 years of postdoctoral studies in Switzerland and the United States, with research interests in SCI and pain. To date, he has made several important contributions to the validation of contact heat evoked potentials (CHEPs), as well as the development of clinical trial endpoints for SCI. Focused on the use of advanced neuroimaging and quantitative sensory testing techniques, his current work aims to better understand changes in the central nervous system related to the development of neuropathic pain. Using large SCI datasets, he is also exploring the relationship between pain, neurological recovery, and other secondary health outcomes.
A new way to monitor bladder health at home
Near Infrared Spectroscopy (NIRS) is non-invasive optical technique that uses light to show changes in blood flow and oxygenation in the body. Dr. Andrew Macnab pioneered the use of NIRS in Canada, starting at Children’s Hospital in 1979.
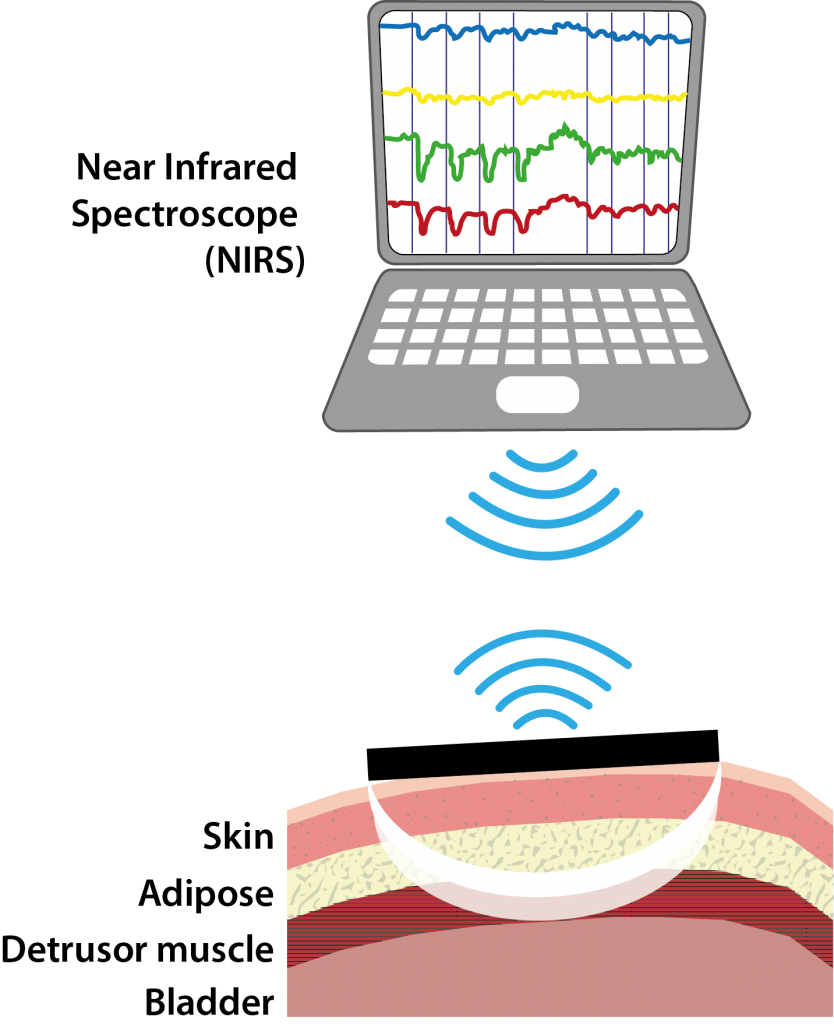 ICORD researcher Dr. Lynn Stothers met Dr. Macnab 10 years ago when they were both working at the Jack Bell Research Centre. They discovered that NIRS could detect changes in blood flow and oxygenation in the bladder as it contracts to pass urine, and that these changes differ depending on whether a patient has a healthy or diseased bladder.
ICORD researcher Dr. Lynn Stothers met Dr. Macnab 10 years ago when they were both working at the Jack Bell Research Centre. They discovered that NIRS could detect changes in blood flow and oxygenation in the bladder as it contracts to pass urine, and that these changes differ depending on whether a patient has a healthy or diseased bladder.
Drs. Stothers and Macnab have since developed a way for patient’s bladder function to be monitored using a small self-contained wireless NIRS system that is taped to the skin over the bladder, and for the past 2 years, wireless bladder monitoring has been done in collaboration with ICORD researchers Drs. Mark Nigro and Babak Shadgan at the Brenda and David McLean Integrated Spine Clinic.
This group have recently also developed a NIRS system that can be used at home and is able to transmit data to the investigators using a cell phone and laptop.
Drs. Macnab and Stothers believe that making it possible for people to check their own bladder health at home is empowering, increases independence, and will provide better quality of life. It also saves time and money for both patients and the health care system, and will be important for people with SCI—with a NIRS monitor patients can check their bladder health every day if they want, without any risk or inconvenience. For example, it will be possible in this way for a patient to have early warning of a possible urinary tract infection without having to make visits to the clinic until the possibility of an infection is detected using the NIRS bladder monitor.
Dr. Stothers, along with Dr. Shadgan and spine clinic urologist Dr. Mark Nigro, are about to start testing a bladder home monitoring system which allows patients to do their own data collection (the same way people can take their own temperature or blood pressure at home). The aim of this Rick Hansen Institute-funded study is to see if regular monitoring of bladder health linked to home video-conferencing between participants and a research nurse is beneficial to people with SCI-related bladder problems. Eligible participants will visit the Urology Clinic in the BSCC for an initial assessment, followed by another clinic visit after 6 months. They will have at least 6 months of monitoring, and weekly video-conferences over the internet with a study nurse, followed by a final study visit at the clinic. Click here for more information about this study, or to see if you’re eligible to participate.
Because NIRS is non-invasive and can be done at home, the technology can be easily extended to developing countries as advances are made in device design. Drs. Macnab, Stothers and Shadgan received a Grand Challenges Canada grant to develop a bladder monitoring system that is inexpensive and can be used by rural health workers in Uganda to screen for early signs of bladder disease, and identify patients who need to receive treatment to prevent their disease advancing:
Using light to detect urinary tract / bladder problems (Canada, Uganda, and Ethiopia). An estimated 2% of deaths in Uganda and widespread chronic illnesses are attributed to urinary tract / bladder problems becoming advanced before they are recognized. Early diagnosis will enable patients to begin treatment before irreversible problems develop and rationalize the use of the scarce resources available to investigate, treat to save organ function, and reduce hypertension. A prototype of an inexpensive NIRS device developed at the University British Columbia for use in rural health clinics in Uganda is being trialed to measure changes in bladder blood flow and oxygenation through the skin as a patient passes their urine. The data are sent by internet link for computer-aided diagnosis at a University centre, and those requiring early treatment are identified. Grand Challenges Canada Grant # 0382-01
 Difference makers royally celebrated
Difference makers royally celebrated
ICORDians Peggy Assinck and Mustafa Hasan were honoured in September with Rick Hansen Difference Maker awards. The awards were presented by Her Royal Highness Sophie, the Countess of Wessex, during a special visit to the Blusson Spinal Cord Centre.
Peggy is a PhD candidate in the Tetzlaff lab. She came to ICORD to do cutting edge SCI research, and is currently working on a project using stem cells derived from skin to treat spinal cord injuries. Peggy also worked with the Krassioukov lab at the Paralympic Cardiovascular Health Clinic at the 2014 Paralympics in Sochi, Russia. In addition to the exhaustive demands of her doctoral training, she also works tirelessly on the ICORD trainee committee and jumps at the chance to support ICORD in the community – including going to Vanderhoof BC to thank the students at WL MacLeod Elementary School for their efforts to raise funds for ICORD’s SCI research. If that weren’t enough, she is also a member of the Canadian Women’s Sledge Hockey team, and hopes to one day compete for Canada at the Paralympics!
Mustafa started as a research participant and volunteer with ICORD, and has recently started working part-time as a research assistant in Dr. Tania Lam’s laboratory. He came to Canada from Iraq several years ago and has volunteered more hours at ICORD than any other volunteer, including his work at the SCI Resource Centre, ICORD research projects, PARC and a variety of other BSCC events and initiatives. He embodies the spirit of this BSCC – the engagement of people with SCI in research (not just as participants but also as contributors and supporters), hard work toward recovery and independence, and the pursuit of innovation (Mustafa has been one of the earliest “test pilots” of our new EKSO robotic exoskeleton, teaching researchers how to use the device with people with SCI and helping to develop a safe research protocol and train new staff in its operation). Mustafa recently competed in his first quad rugby tournament, for which the entire Lam Lab showed up to cheer him on.
Dr. Brian Kwon leads collaborative study on biomarkers
A study led by ICORD Principal Investigator Dr. Brian Kwon is bringing together a team of world-class investigators from multiple disciplines to create a better understanding of SCI, potentially leading to advances in the treatment of paralysis.
Currently, the severity of spinal cord injury is assessed using the ASIA Impairment Scale, which is based on how much sensation a patient reports, as well as their motor function. This assessment can be difficult to perform if a patient is badly injured or under the influence of alcohol or drugs. “Right now, assessing the severity of spinal cord injury and prognosticating outcomes is done through functional testing, which can be very vague and does not offer precise measures for how to predict those outcomes,” says Dr. Kwon, who is also an orthopaedic spine surgeon at Vancouver General Hospital.
Dr. Kwon’s three-year study, “Biomarkers for Crossing the Translational Divide in Acute Spinal Cord Injury” recently received $3-million in funding from Brain Canada as a Multi-Investigator Research Initiative (MIRI) grant. The research team includes experts from the University of British Columbia, University of Victoria, University of Alberta, the PROOF Centre of Excellence, the Translational Genomics Research Institute and the Rick Hansen Institute, in addition to a team of spine surgeons across Canada.
 “We have a great team of spine surgeon collaborators at centres across Canada who are collecting extremely valuable samples of spinal fluid and blood from patients who have had an acute SCI,” says Dr. Kwon. “To get the most of these samples we will employ very complex analytical platforms, and having world-class expertise at all of those levels is key. Nobody else in the world has this collection of human samples, so we want top-level people doing the analysis.”
“We have a great team of spine surgeon collaborators at centres across Canada who are collecting extremely valuable samples of spinal fluid and blood from patients who have had an acute SCI,” says Dr. Kwon. “To get the most of these samples we will employ very complex analytical platforms, and having world-class expertise at all of those levels is key. Nobody else in the world has this collection of human samples, so we want top-level people doing the analysis.”
The study has three objectives: first, to expand currently limited knowledge of what is actually happening biologically in the spinal cords of human SCI patients; second, to establish biomarkers that identify severity of injury to the spinal cord; and third, to create biomarker linkages with an intermediary model where novel therapies can be developed for eventual human clinical trials.
“Investigating what is really going on in the human spinal cord after injury, establishing biomarkers of injury, and developing a useful intermediary model would advance our field’s efforts to more effectively develop and validate novel therapies for SCI, ” explains Dr. Kwon. “We’re trying to establish the pipeline to help facilitate the evolution of treatments from bench to bedside.”
Dr. Kwon received additional funding of US$53,000 for this project from the organization Unite2FightParalysis at their recent Working 2 Walk Symposium in Seattle.
WHAT IS A BIOMARKER? A “biomarker” is a molecule that can be used to measure specific biological processes or assess aspects of a person’s health. In this case, Dr. Kwon’s study is using biomarkers to measure the severity of spinal cord injury.
 SCI in the news
SCI in the news
[reprinted from the SCRIBE Blog on the ICORD web site] A BBC story about a man with SCI who can walk again after receiving a new therapy was in the news lately. The story reports that Darek Fidyka, a 40-year-old Polish man who sustained a spinal cord injury during a stabbing, had olfactory bulb cells from his nasal cavity transplanted into his spinal cord, and two years following this treatment (and extensive rehabilitation), he is able to walk with a walker. There is a lot of excitement in the media about this new treatment, conducted in Poland and pioneered by British researcher and physician Dr. Geoffrey Raisman.
While this research is very interesting, ICORD Director Dr. Wolfram Tetzlaff has some concerns.
“This is a study with one patient only, so I believe it is premature to draw conclusions. It’s important to do a large-scale clinical trial with blinded assessors before we can know for sure whether the transplantation surgery will be a viable treatment for SCI,” said Dr. Tetzlaff, who was asked for comments by several news outlets on October 21st. “This patient presented as having a complete SCI, but he had a 2mm “bridge” of spared tissue at the site of injury. These bridges can be non-functional when compressed by scarring. It’s possible that the surgery done to remove the scar tissue before transplanting the olfactory cells (known as “untethering“) might have decompressed the bridge, allowing it to function again.”
“In addition this patient received extensive physiotherapy (5 hours daily/5 days a week) for 8 months before and 21 months after his surgery. He showed modest but significant motor recovery by 11 months after surgery, and this rehabilitation regimen likely contributed to the recovery seen by the patient. For these reasons alone, it is impossible to conclude presently whether these cells and bridges had an effect. The MRI performed 19 months post-treatment showed no new nerve fibres in the lesion site, suggesting this was not a regeneration effect,” Dr. Tetzlaff continued.
“We hear similar anecdotal reports from our colleagues in China, who are fortunate to have the resources to provide 6 hours of rehab/6 days a week (with the help of family members living in or near the hospitals). What this indicates is that some functionally complete patients would likely benefit from more extensive and longer rehabilitation than is presently offered. We do know that apart from initial stabilization surgery, rehabilitation is currently the only effective treatment for SCI, although there are therapies currently available to improve the quality of life of people living with SCI. Sadly, this media hype makes other people living with SCI wonder if they should try to get this new treatment right away. I really feel that it’s important for people to remember that any risky intervention like this, involving two separate surgeries, needs validation in a clinical trial,” he said.
“What it should leave us with is the hope that indeed improvements are possible, even in cases deemed ‘complete,’” said Dr. Tetzlaff. “I feel strongly that with more funding, incremental steps towards more effective treatments will happen.”
Find out more:
See the CTV news report | See the CBC News report | Read SCI-BC’s blog post on this topic. | Read this important document about the risks and potential benefits of participating in clinical trials. | Read the scientific paper in Cell Transplantation. Note: this link may require academic library access. For assistance, please visit the Community Resource Centre in the atrium of the Blusson Spinal Cord Centre.
The view from the bench
(a grad student’s perspective)
By Jessica Inskip (@jessinskip), PhD Student in Dr. Victoria Claydon’s Lab at Simon Fraser University
In this fall time of year, it’s not just grade-schoolers who get that mixed back-to-school feeling! As Graduate Students, we often mark the years that we have been at graduate school with the number of times September has come around. The new school year is a time for revising and updating our goals, starting a fresh calendar, getting new school professional clothes and maybe even a haircut.
I hope this year I had my last back-to-school haircut.
As graduate students, we walk a line between professional and student – neither quite here nor there: part student, part research professional, rarely glamorous. From this position, it can sting a little when our friends and family ask about our day at “school” – whether or not there is a hint of mockery in the question. So, what to ask the graduate students you meet around the building instead? Ask us how our research is going; what we are excited about these days; what have we read lately that’s interesting? For all of our sakes, just steer clear of asking how many Septembers we’ve been here!
Dance showcase: entertaining and educational!

Some highlights from the show. Left: William Wu and Kirsten Sharp; right: Alisa Popok and Kyle Gieni
The Shall We Dance showcase on October 6th was a great success. Thank you to all the dancers: Zika Trajkovic & Scarlett Liaifer, Aleksander Vlasev & Victoria Zhu, Mathew & Melanie Chung, William Wu & Alisa Popok, Kyle Gieni, Jessica Kruger, Kirsten Sharp, and David. This was an amazing show and we hope it was just the first of many! Organizer Alisa Popok is now planning some wheelchair dance workshops. If you’re interested, let us know.
Don’t miss the gala!
You still time to get your tickets to the 6th annual Spinal Chord Gala, coming up on November 1st. This fun event is jointly-hosted by ICORD and the Vancouver Cantata Singers. At ICORD, we use gala funds to support equipment grants for researchers, staff awards for service and research, the SCI Community Resource Centre and PARC. Tickets are $100 each (with an $80 tax receipt) and are available from the ICORD Admin Office (cash, cheque or Visa/Mastercard accepted) or online.
Partner news
 Spinal Cord Injury BC is excited to announce the launch of a new online video series, SCI BC TV. Through its mini-documentary format, SCI BC TV motivates viewers to realize their potential, remove perceived barriers and open their minds to new experiences and information. By surprising and educating the public, this YouTube show attempts to eliminate stereotypes, common misconceptions and the often miscommunicated “Wow, you can do that?” reaction. Our bi-monthly episodes cover informative, edgy topics, integrated with humour and human connection. Take a look!
Spinal Cord Injury BC is excited to announce the launch of a new online video series, SCI BC TV. Through its mini-documentary format, SCI BC TV motivates viewers to realize their potential, remove perceived barriers and open their minds to new experiences and information. By surprising and educating the public, this YouTube show attempts to eliminate stereotypes, common misconceptions and the often miscommunicated “Wow, you can do that?” reaction. Our bi-monthly episodes cover informative, edgy topics, integrated with humour and human connection. Take a look!
 Rick Hansen Institute has just launched a new resource website for spinal cord injury. Supporting Clinical Initiatives in Spinal Cord Injury or SCI2 contains resources and tools developed by experts from across the country on topics such as skin integrity, walking mobility, respiratory function and much more. In collaboration with members of the sexual health clinic at Vancouver Coastal Health, there are also a number of resources for individuals with SCI on fertility, pregnancy and sexuality.For members of a Rick Hansen SCI Registry facility, SCI2 also provides access to facility reports which give simple, actionable information about each of the clinical areas on the site. The reports also show how patients change over time and how they compare to patients across the country. The site includes resources to help support the integration of a new or modified practice such as clinical practice guidelines and examples of assessments. Visit SCI2.
Rick Hansen Institute has just launched a new resource website for spinal cord injury. Supporting Clinical Initiatives in Spinal Cord Injury or SCI2 contains resources and tools developed by experts from across the country on topics such as skin integrity, walking mobility, respiratory function and much more. In collaboration with members of the sexual health clinic at Vancouver Coastal Health, there are also a number of resources for individuals with SCI on fertility, pregnancy and sexuality.For members of a Rick Hansen SCI Registry facility, SCI2 also provides access to facility reports which give simple, actionable information about each of the clinical areas on the site. The reports also show how patients change over time and how they compare to patients across the country. The site includes resources to help support the integration of a new or modified practice such as clinical practice guidelines and examples of assessments. Visit SCI2.
Coinciding with the launch of the SCI2 resource website, RHI has published the Rick Hansen SCI Registry Special Report 2011-2013 which includes data on areas such as demographics, level and severity of injury, length of stay in acute and rehab care and social impacts post-injury such as income, marital status and employment. View the report on the SCI2 website.
About this issue’s cover:
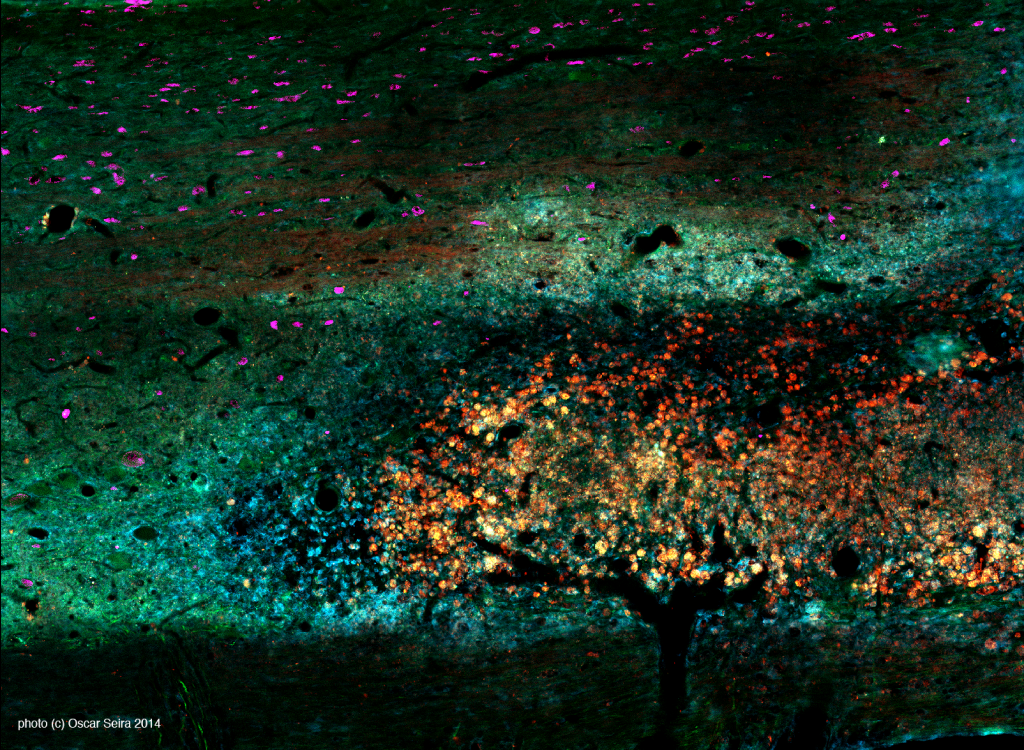 Our cover image and its description were contributed by Dr. Oscar Seira, a Postdoctoral Fellow in Dr. Wolfram Tetzlaff’s laboratory.
Our cover image and its description were contributed by Dr. Oscar Seira, a Postdoctoral Fellow in Dr. Wolfram Tetzlaff’s laboratory.
Fall Evening Landscape
The coming of fall is inevitable . . . so inevitable that it even wants to be present at microscopic level in our research, as you can see in this picture!
The image shows a thin section of a rodent spinal cord which was injected with modified Lipid Nanoparticles with the final aim of promoting axon regeneration. These nanoparticles (shown in red) spread within the spinal cord, looking like fall foliage over a dark branches. In blue we can appreciate the inflammatory response against the nanoparticles, also calling to mind a late autumn evening, chilly and quiet. Finally, motoneurons (shown in pink) appear in the darkness of the sky like little stars.
[click the image to enlarge]





