A key challenge in treating traumatic spinal cord injury (SCI)—the kind caused by impact from a car crash, a fall, a sporting activity or a violent act—is repairing the gap that is formed when the spine is broken.
This gap, typically a few centimetres wide, essentially blocks nerve impulses from getting through, leading to serious health issues that may include paralysis, loss of blood pressure, bladder and bowel control, sexual dysfunction, and chronic pain.
Now a new, multidisciplinary team—aptly named Mend the Gap—is working on a novel approach that may help people with SCI.
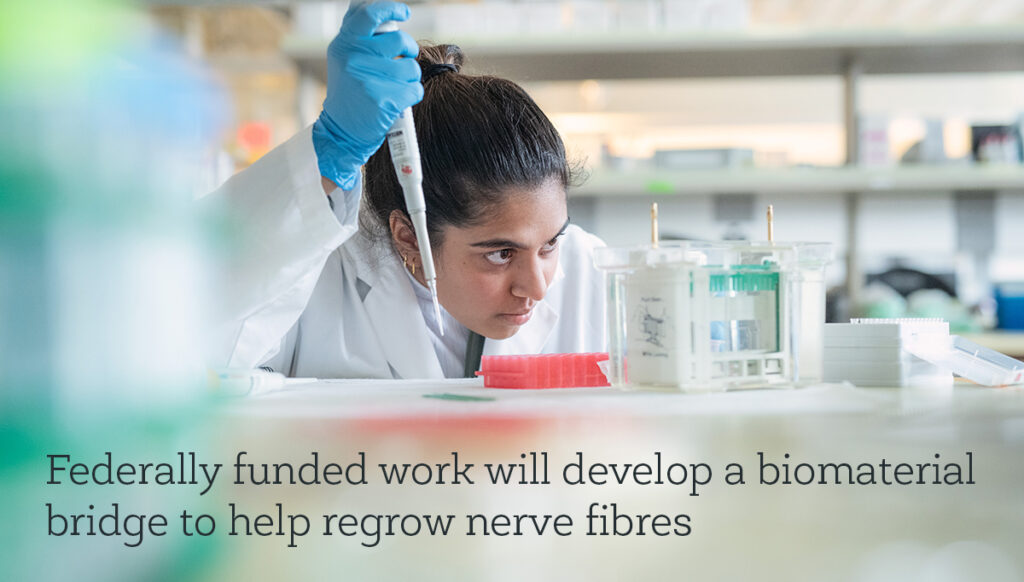
The Mend the Gap team, which includes ICORD researchers Drs. Wolfram Tetzlaff, Brian Kwon, Dena Shahriari, Michael Berger, Corree Laule, Babak Shadgan, andStephanie Willerth, recently received $24 million from Canada’s New Frontiers in Research Fund 2020 Transformation stream to investigate using biomaterials—and soft gels in particular—to heal the injury.
The soft gel will be injected into the site of the injury to serve as a bridge for growing nerve fibres.
“A biomaterials bridge is compatible with other systems and structures in the body and is minimally disruptive,” explains principal investigator Dr. John Madden, a professor of electrical and computer engineering in the faculty of applied science at the University of British Columbia.
“The soft gel that our team plan to use contains tiny magnetic rods that are aligned using an external magnet, creating guide rails that support the nerve fibres to grow in the right direction, eventually crossing the gap.”
Personalized, less invasive treatment
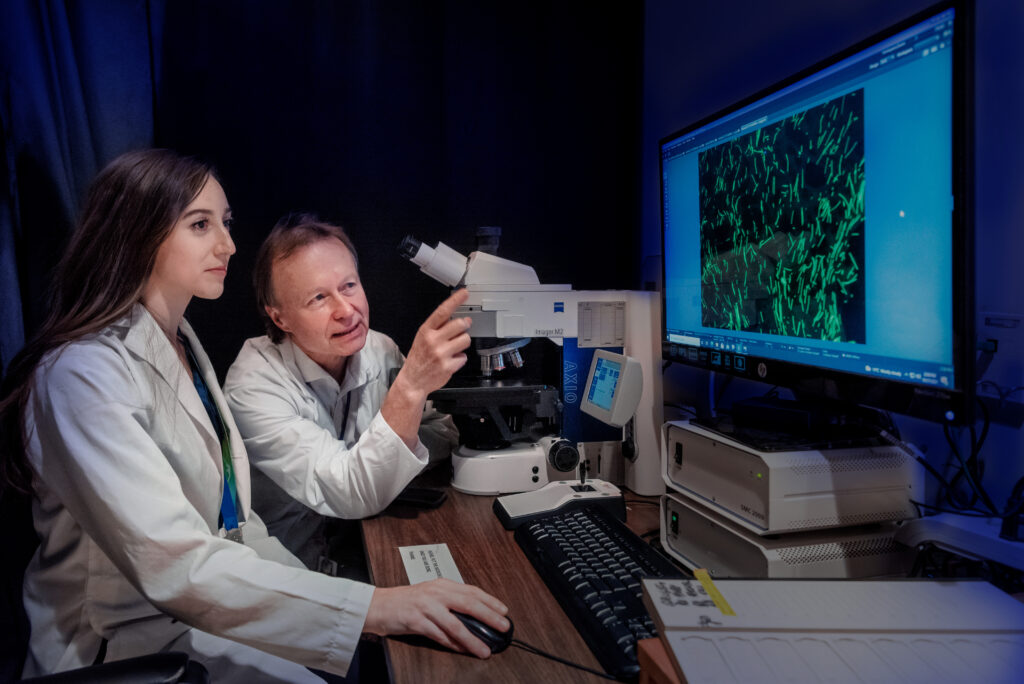
Previous treatments for spinal cord injuries used solid bridges, which have the drawback of risking injury to any remaining healthy nerve fibres and bodily functions, explains co-principal investigator Dr. Wolfram Tetzlaff, a professor of surgery and zoology at UBC and director of ICORD, a world-leading centre for spinal cord injury research within the UBC faculty of medicine and the Vancouver Coastal Health Research Institute.
“A soft gel can be moulded into the shapes of the many different lesions seen in the body, and thus provide personalized treatment,” said Dr. Tetzlaff. “Since the surgery will be minimally invasive, we can potentially see shorter recovery times and minimal damage to the patients.”
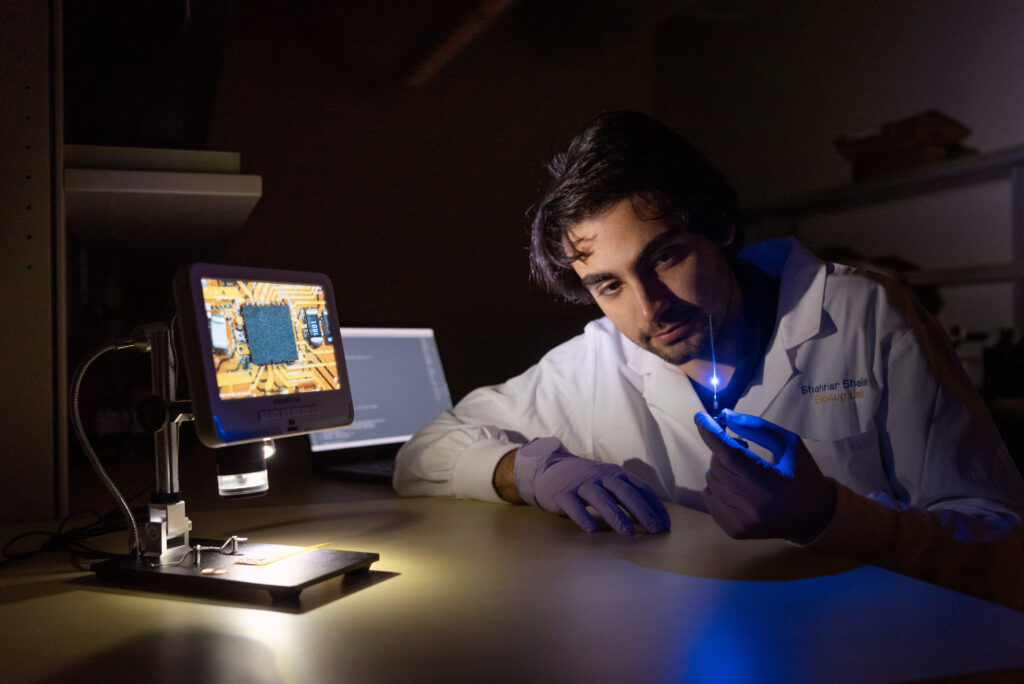
Co-principal investigator Dr. Dena Shahriari adds that thus far, research in SCI has been largely focused on biomaterials that need to be implanted through invasive surgery.
“Here, we shift the focus to injectable biomaterials to potentially protect any residual function that those living with SCI heavily rely on and treasure,” says Dr. Shahriari, a biomaterials scientist and neural engineer, and an assistant professor at UBC’s department of orthopaedics and school of biomedical engineering. She also leads a team at ICORD that develops neuroelectronic devices, sensors and smart biomaterials to interface with biological tissues and provide new capabilities for tissue regeneration and improving organ function.
One reason repairing the spinal cord is so difficult is the presence of scar tissue, so the soft gel will contain drugs that can modify that tissue and revive the nerve fibres. The gel will be injected into the spinal cord by a machine-vision-equipped surgical robot for enhanced precision.
“Every week we admit a new patient whose life has been turned upside down after suffering a spinal cord injury,” says co-principal investigator, Dr. Brian Kwon, a professor of orthopaedics at UBC’s faculty of medicine and ICORD PI.
“It serves as a stark reminder that we have to be pushing the boundaries of science and innovation in initiatives like Mend the Gap to establish novel ways of repairing the injured cord.”
Spinal cord injuries cost Canada at least $3 billion a year, about a third of the cost of all cancers.
And while the primary goal of Mend the Gap is repairing the spinal cord in recently injured individuals, the team does not rule out eventually applying the results to those who have chronic injuries in the future.
Where science, engineering, medicine and ethics meet
The 32-member project includes researchers, engineers and surgeons from Canada, the United States, Europe and Australia. In Canada, the network includes UBC, ICORD, the University of Alberta, University of Western Ontario, McGill University and University of Toronto.
Co-principal investigator Dr. Karen Cheung says the project highlights the unique advantages of bringing together medical and engineering knowledge to tackle the complexity of spinal cord injuries.
“Biomedical engineers play a central role in addressing grand challenges in health, because they analyze, interpret, transform and recombine knowledge and information from all of these domains—materials engineering, electrical engineering, neuroscience, chemistry, physics—to generate new technologies and make impactful discoveries,” says Dr. Cheung, a bioengineering professor at UBC’s school of biomedical engineering.
Key to the journey, adds co-principal investigator Dr. Judy Illes is the integration of the voices and values of patients themselves and the people in their families and surrounding networks.
“With their input, Mend the Gap will be able to maximally target short- and long-term goals that are prioritized by those most affected by SCI and get results beneficially back out to them,” says Dr. Illes, who is also co-chair of the project’s ethics and knowledge translation council with athlete and activist Rick Hansen. The council helps ensure alignment between the research objectives and the needs of those with spinal cord injury.
At this point, finding a “cure” for SCI is not the project’s goal as the central nervous system is just too complicated, says Dr. Tetzlaff, adding the key technology needed for this will be developed over the next six years. “Ultimately, we hope to see increased motor function, a longer life span and a better quality of life for SCI patients and their families.”
This article originally appeared, in slightly different form, on news.ubc.ca
Photos by Martin Dee